Pancreatitis, inflammation of the pancreas, is a rather dangerous disease that significantly worsens people's quality of life. And an important component of the correct treatment of this unpleasant disease is considered proper nutrition, which has a beneficial effect on the functioning of the organ. What should be the diet for pancreatitis - read in our material.
Don't self-medicate: in our articles we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can make a diagnosis and prescribe treatment. We want to help those who are faced with diseases of the pancreas (by the way, among office workers and former students, pancreatitis ranks third "in popularity") and therefore we have collected in this article the basic recommendations on the diet for pancreatitis and cholecystitis. We have also prepared sample menus and several useful recipes. Read it, it will be useful to you!
What is pancreatitis
Pancreatitis is an inflammation of the pancreas, which participates in the digestion process and also regulates metabolism. This is a "2 in 1" organ, it has a complex structure: the bulk of the gland secretes the enzymes necessary for digesting food in the intestine, and the so-called "pancreatic islets" are an endocrine organ that produces the hormone insulin.
When the pancreas becomes inflamed, the release of enzymes into the duodenum stops. As a result, these aggressive substances are activated in the gland itself and begin to destroy it - this process is often called autodigestion. This releases toxins that travel through the bloodstream to other organs and can damage them. Pancreatitis can be acute or chronic.
Acute inflammation of the pancreas
Acute pancreatitis is a dangerous disease that requires immediate treatment, usually in a hospital setting. Most often it occurs due to alcohol abuse or gallstone disease, when a stone blocks the duct. The disease is characterized by severe pain in the upper abdomen, sometimes radiating to the back; nausea; vomit; general worsening of conditions.
Chronic pancreatitis
With chronic inflammation of the pancreas, the organ is gradually destroyed. The main causes of the disease are alcohol consumption and smoking. The most typical manifestation is abdominal pain, which usually occurs after eating. The lack of digestive secretion from the pancreas leads to the fact that food is poorly digested, flatulence and bloating occur. There is often no appetite and weight may decrease.
Symptoms of pancreatitis
The main symptom of acute and chronic inflammation of the pancreas is pain in the upper abdomen. Often such pains are excruciating. In the chronic form, heaviness in the stomach, nausea and stool disorders are often observed. Unpleasant sensations make pancreatitis suspected, and then the diagnosis is confirmed with the help of tests and other studies.
Why do you need a diet for pancreatitis (inflammation of the pancreas)?
The diet for pancreatitis in adults is designed to reduce the load on the affected organ so that it can recover. In acute pancreatitis it is also important to reduce enzyme synthesis to stop the process of destruction of the gland.

Diet principles for pancreatitis
- Refusal of any food that causes the production of enzymes: smoked, spicy, pickled, fried.
- Food should be warm (not cold or hot), mushy.
- Meals should be fractional, portions should be small.
- The main emphasis in the diet is on protein products: up to 200 grams should be consumed per day. But fats and carbohydrates are significantly limited.
- The amount of salt is reduced to 3-5 grams; foods are not salted during cooking.
- Raw foods are excluded. It is not possible to consume fresh fruit and vegetables, only boiled or baked.
- Carbohydrates should be consumed in moderation, but foods containing sugar should be limited.
What should be the diet for acute pancreatitis?
The diet for acute pancreatitis is as strict as possible: the menu on the first day does not include food, only water. After a few days you can eat small portions of liquid food: vegetable broths and purees, boiled porridges, mucous decoctions, liquid meat purees. You can gradually expand the range of dishes using permitted products.
Diet for chronic pancreatitis
The dietary menu for chronic pancreatitis is more varied, but it is recommended to follow it for a long time, at least six months. It is believed that during this period not only the condition of the pancreas will improve, but the patient will also wean himself from all kinds of harmful foods, such as fried, smoked and pickled foods.
Traditionally, for chronic pancreatitis, the diet "Table No. 5p" is prescribed. The system of dietary tables was developed in the 1920s, and although it has now been abandoned, many doctors still recommend adhering to the principles of such diets.
The diet "Table No. 5" is prescribed for pancreatitis and cholecystitis, but especially for the restoration of the pancreas a special version of this diet is recommended: "Table No. 5p". It is distinguished not only by a reduced amount of fat in the diet, but also by the limitation of carbohydrates. It is necessary to consume a lot of proteins: proteins are necessary for the rapid restoration of pancreatic tissue.
The diet for exacerbation of pancreatitis is more rigorous, it is formed in the image and likeness of the diet recommended for the acute form of the disease. Pureed food, divided meals, avoiding salt and spices will help you deal with the disease faster.
What you can eat if you have pancreatitis (inflammation of the pancreas)
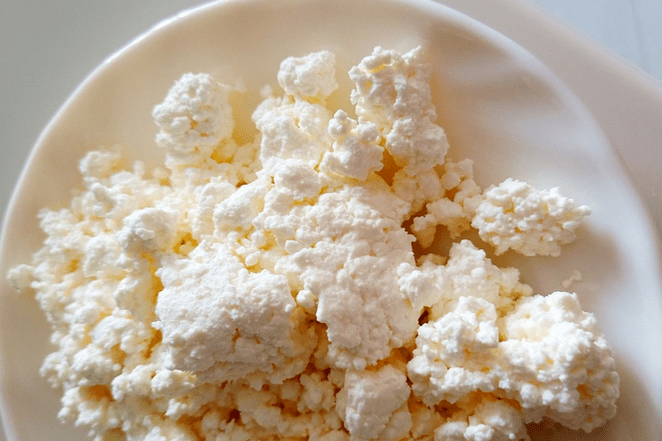
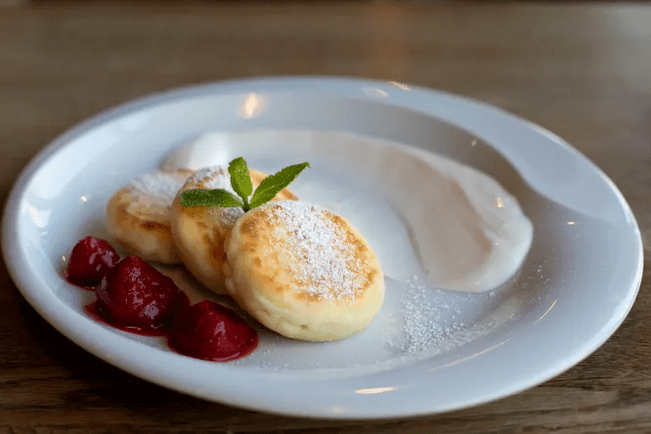
So, it's time to figure out what you can eat during a pancreatitis diet to recover quickly and avoid painful attacks. We remind you that the list of permitted products varies depending on the stage of the disease. During flare-ups it is recommended to fast and eat a very limited range of foods, but during the remission period many more foods are allowed. Low-fat cottage cheese occupies an important place in the diet of those suffering from pancreatitis.
- lean meat (veal, chicken, turkey, rabbit and even lean pork are suitable);
- lean fish (pike, cod, flounder, cod);
- low-fat cottage cheese, low-fat and mild cheese;
- eggs in the form of a steamed omelette made from egg whites (you cannot eat more than one yolk per day);
- low-fat fermented milk products;
- milk – only low-fat, if tolerated;
- cereals (semolina, rice, oatmeal, buckwheat);
- stale bread, inedible crackers;
- pasta;
- boiled or baked vegetables (potatoes, beets, carrots, courgettes, pumpkin);
- boiled or baked sweet fruit (apples, bananas, pears);
- dried fruit;
- jelly, jam, honey, jelly - in small quantities.
The list of what you can eat on a diet for pancreatitis is not so short: if you wish, you can easily do without violations, being content with only the permitted foods for a long time. It is worth considering that the recommendations were developed 100 years ago and many new products have appeared since then. They can be added to the menu with caution if they contain a lot of protein and little fat, such as boiled squid.
What not to eat on a pancreatitis diet
The pancreatitis diet prescribes serious restrictions to the menu, but you can expect improvement in the condition only if you strictly follow them. The following foods cannot be included in diet menu no.
- legumes (the only exception is green beans in moderation, boiled or stewed);
- onions, garlic, radishes, radishes, peppers and other spicy vegetables;
- spinach, sorrel, fresh herbs;
- all kinds of cabbage;
- mushrooms;
- sour fruit;
- marinades and pickles;
- carbonated drinks, packaged juices (it is also better not to drink fresh juices);
- alcohol;
- coffee and cocoa;
- ready sauces, mayonnaise;
- Fast food;
- fresh bread, baked goods;
- any confectionery products;
- ice-cream;
- fatty meat and fish;
- sausages and delicacies;
- caviar;
- canned food;
- smoked meats;
- meat, fish and mushroom broths.
With an exacerbation of pancreatitis of the pancreas, the diet becomes even more strict, and even those foods that can be safely included in the diet during remission can be included in the list of prohibited foods. Here you need to listen to the recommendations of your doctor.
Diet for chronic pancreatitis (inflammation of the pancreas): sample menu for a week

We present an approximate diet for chronic pancreatitis for a week. This is not a dogma, but simply a guideline for those who want to restore the pancreas with proper nutrition.
Monday
- Breakfast: a sandwich of stale bread with low-fat cheese, a bowl of porridge with water or diluted milk.
- Second breakfast: a portion of low-fat ricotta with dried fruit.
- Lunch: vegetable soup, steamed beef cutlet with mashed potatoes in water with a small piece of butter.
- Afternoon snack: cooked apple.
- Dinner: boiled lean fish, steamed vegetables allowed.
Tuesday
- Breakfast: oatmeal with water
- Second breakfast: baked sweet apple puree
- Lunch: vegetable cream soup, steamed chicken breast; berry jelly.
- Afternoon snack: low-fat yogurt.
- Dinner: steamed omelette with vegetables.
Wednesday
- Breakfast: cottage cheese casserole with dried fruit
- Second breakfast: bananas
- Lunch: rice and vegetable soup; steamed rabbit meatballs, compote.
- Afternoon snack: apple jelly, biscuits.
- Dinner: steamed fish, vegetable puree.
Thursday
- Breakfast: rice porridge, soft-boiled egg.
- Second breakfast: yogurt, cooked apple.
- Lunch: soup with pasta; Fish balls with vegetable puree.
- Afternoon snack: low-fat cheese sandwich.
- Dinner: lazy ricotta dumplings, a little sour cream.
Friday
- Breakfast: cottage cheese with a spoonful of honey or jam.
- Second breakfast: steamed egg white omelette.
- Lunch: mashed potato soup, baked beef with steamed vegetables, jelly.
- Afternoon snack: dried fruit compote.
- Dinner: lean fish quenelles, rice.
Saturday
- Breakfast: semolina porridge, soft-boiled egg
- Second breakfast: yogurt.
- Lunch: fish soup with rice, stewed rabbit with potatoes, compote.
- Afternoon snack: ricotta casserole.
- Dinner: cheese sandwich, steamed protein omelette.
Sunday
- Breakfast: buckwheat porridge.
- Second breakfast: cooked apple.
- Lunch: pumpkin cream, steamed beef cutlets, pasta.
- Afternoon snack: jelly, biscuits.
- Dinner: cottage cheese, boiled vegetables.
Diet for the pancreas: recipes
Despite the limited range of products, the diet for pancreatitis can be quite varied. We offer some ideas for inspiration.

Ingredients:
- Rice in bags;
- Potato;
- Carrot;
- Pumpkin;
- Salt.
Preparation: prepare the rice water: cook the rice in a pan with plenty of water, then remove the bags. Grate the carrots, chop the remaining vegetables, put everything in a pan with rice water, add rice there, cook until the vegetables are ready. Salt, mix, turn off. If necessary, grind everything in a blender.
Fish quenelles
- Lean fish fillet;
- White crackers;
- Milk;
- Egg white;
- Salt.
Preparation: grind the fish in a meat grinder, soak the crackers in milk, also pass through the meat grinder, mix with the chopped fish. Beat the egg white until frothy, add it to the minced meat, add salt and mix. Form round quenelles with the resulting minced meat. Then boil or steam them.
Pumpkin puree soup with oatmeal
Ingredients:
- Pumpkin;
- Potato;
- Hercules;
- Cream;
- A little oil for stewing.
Preparation: cut the pumpkin and potatoes, simmer them in a deep bowl with a drizzle of oil, taking care that they do not burn. Season with salt, add the oat flakes, add the water, mix, leave to simmer until the oat flakes are ready. Puree the contents of the pan through the blender, return it to the pan, add the cream and leave to simmer for a few more minutes. It can be served with breadcrumbs.
According to reviews, it is not very easy to follow a diet for pancreatitis, at least in the phase of pureed food, but with its help you can achieve a truly stable remission. Patients note that they feel much better on such a diet.
Results of treatment of chronic pancreatitis with diet
In case of chronic pancreatitis, the diet is prescribed not for a week or a month, but for at least six months. It is more often recommended to limit yourself to foods harmful to life, so as not to provoke an exacerbation.
Together with other treatment methods, a diet for the pancreas has a beneficial effect on the organ and promotes its rapid recovery. The longer no exacerbations occur, the bolder you can expand your diet for pancreatitis, including all new products.
In some cases, the pancreas is completely restored thanks to timely treatment and diet, so after the end of therapy it is possible to return to the usual eating style. However, it is better to abandon unhealthy habits and choose PP dishes even after complete recovery.
It is impossible to count the number of different diets. Some of them are prescribed for therapeutic purposes and others are aimed at reducing body weight. Human nutrition, like any other organism, affects its health, since the composition of food and the saturation of necessary vitamins and microelements determine the possibility of having a normal physiology. Any restrictions, both in composition and quantity, inevitably affect our organism. Each disease has its own mechanism of development, and, accordingly, nutrition should also be different.
The pancreatitis diet is aimed at reducing inflammation in the pancreas. The sooner you start following it, the better results you can expect. In the acute phase, fasting can be used, but it usually does not last more than two or three days. Next, foods with maximum fat restriction are introduced smoothly. Lean varieties of skinless meat and poultry (veal, lean beef, chicken, rabbit, turkey, etc. ) are suitable. Buckwheat, barley, mashed potatoes, stewed vegetables can be used as a garnish. Fried, spicy, salty foods, baked goods, refractory fats (lamb, pork, goose, duck, fatty beef, poultry skin, margarine, mayonnaise) can contribute to a new exacerbation.
The use of additional enzyme therapy will improve the condition. Minicrosphere and microtablet preparations are more effective. The usual dose is around 25, 000 units. The diet described above has the right to exist, but if its use is justified and is followed only for a short period of time. Stabilization of the condition with pancreatitis is an indication for a planned and gradual expansion of the diet.































